Specialties & Procedures
As a top spine surgeon in Manhattan, Jun S. Kim, MD performs a number of different types of spine operations. His speciality is in spinal deformity (scoliosis, kyphosis, adolescent idiopathic scoliosis, Scheuermann’s kyphosis, kyphoscoliosis) and cervical spine surgery. He also performs minimally invasive spine surgery in the right patient for the right indications. In many cases, he finds that his patients ultimately do well without surgery and never need an operation. He believes it is imperative that all non-surgical avenues be explored and trialed before surgery is considered, as all surgery comes with inherent, unavoidable risks. If he isn’t confident that he can help your problem with surgery, then he will not recommend it. Lastly, if and when surgery becomes necessary, Dr. Kim believes the surgery should be personalized and tailored to the individual patient.
- Adolescent Idiopathic Scoliosis Correction
- Adult Idiopathic Scoliosis Correction/ Adult Deformity Surgery
- Corpectomy
- Cervical Spine Deformity Correction
- Decompression/Laminectomy
- Disc Replacement
- Cervical Foraminotomy
- Cervical Laminoplasty
- Microdiscectomy
- Minimally Invasive Spine Surgery
- Endoscopic Spine Surgery
- Spinal Fusion
- Scheuermann’s Kyphosis Correction
- Kyphoscoliosis Correction
Adolescent Idiopathic Scoliosis Correction
Adolescent idiopathic scoliosis (AIS) is the most common form of scoliosis. It affects children between the ages of 10 and 18 years old. The incidence of scoliosis is 3% for curves between 10 and 20 degrees. 0.3% for curves greater than 30 degrees. Larger curves (>30 degrees) are more often found in females (10:1 female to male). The majority of patients with AIS are otherwise healthy and have no medical issues. When the severity of the scoliosis reaches a threshold, Dr. Kim may recommend adolescent idiopathic scoliosis correction surgery.
How Can Adolescent Idiopathic Scoliosis Be Treated?
AIS can be treated non-operatively with close observation or bracing. The goal of non-operative treatment in AIS is to prevent curve progression and, ultimately, surgery. Bracing is the mainstay of non-operative treatment for curves greater than 20 to 25 degrees. A seminal study titled “Bracing in Adolescent Idiopathic Scoliosis Trial”, otherwise known as BrAIST, demonstrated 72% success in preventing curve progression to >50 degrees in patients with curves between 20 and 40 degrees when a brace was worn for at least 18 hours a day.
For a patient with scoliosis, physician visits for clinical evaluation should be scheduled at the following intervals:
- For patients 0–5 years of age with congenital scoliosis: every 3 months
- For patients 6–12 years of age with early onset scoliosis: every 4 months
- For patients 13–18 years of age with AIS, Risser Stage 0–1: every 3 months
- For patients 13–18 years of age with AIS, Risser Stage 2–3: every 4 months
- For patients 13–18 years of age with AIS, Risser Stage 4–5: every 6 months
- For patients 19–30 years of age with AIS, Post-growth surveillance: every 24 month
In cases where the curve progresses to greater than 45-50 degrees, then Dr. Kim may recommend a scoliosis correction and spinal fusion procedure. He will measure and analyze your curve to offer you the most optimal correction and a lasting solution.
Adult Idiopathic Scoliosis Correction/ Adult Deformity Surgery
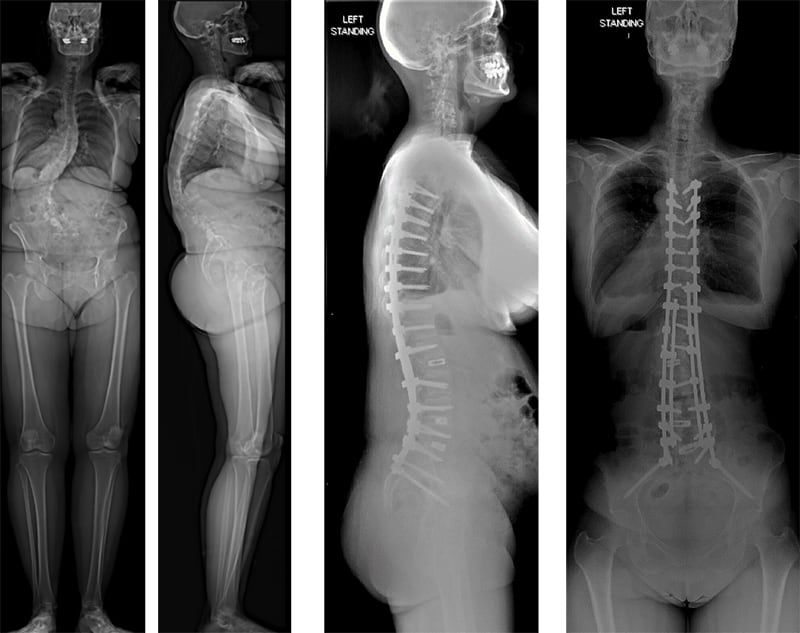
Adult idiopathic scoliosis (AdIS) refers to patients with adolescent idiopathic scoliosis (AIS) over the age of 18. In other words, adult idiopathic scoliosis is a chronological progression of AIS or adolescent idiopathic scoliosis. Adult patients differ significantly from their pediatric counterparts in terms of symptoms, radiographic findings, and surgical treatment. Curves tend to be less flexible and there tends to be significant degeneration of the lumbosacral curve otherwise known as the fractional curve that causes varying degrees of leg pain in addition to back pain.
(Lin et al. Spinal deformity surgery 2021)


Corpectomy
Corpectomy is the surgical removal of all or part of the vertebral body.
Cervical Spine Deformity Correction
Cervical spinal deformity (CSD) in adult patients is a relatively uncommon yet debilitating condition with diverse etiologies and clinical manifestations. Similar to thoracolumbar deformity, CSD can be broadly divided into scoliosis and kyphosis. Severe forms of CSD can lead to pain; neurologic deterioration, including myelopathy; and cervical spine–specific symptoms such as difficulty with horizontal gaze, dysphagia, and dyspnea.

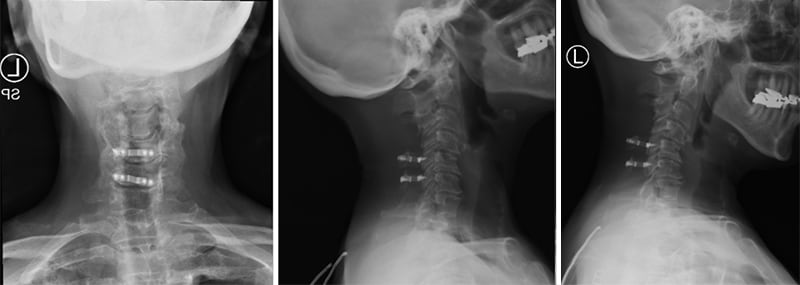
Preoperative rigid cervical kyphotic deformity after sustaining a motor vehicle accident.

Postoperative s/p anterior-posterior decompression fusion
Decompression/Laminectomy
Decompression surgery (laminectomy) is an operation for removal of part or all of the lamina of a vertebra in order to relieve pressure on the spinal cord or nerve roots. The pressure may result from fracture fragments, disc fragments, bone spurs, tumors, or infections.
Disc Replacement
Cervical disc replacement is a motion preserving surgery that is indicated for cervical radiculopathy (nerve compression causing pain radiating to the arm or scapula) and/or myelopathy (spinal cord compression causing imbalance, clumsiness, loss of dexterity). There are several different kinds of replacement discs available in the USA. Dr. Kim prefers the Prestige™ LP. This is because: 1) the earliest version of his disc was first implanted in 1991, so it has the longest track record and 2) it is made of a titanium-ceramic composite that the company claims has demonstrated slower wear while minimally degrading the ability of MRI scans to assess the spine after surgery. The best candidate is someone who has minimal to no arthritis, usually younger than 45, has little to no disc height loss, no arthritis of the facet joint, no bone forming diseases, no inflammatory arthritis (e.g., rheumatoid, lupus, etc.), no infection, and has a stable spine.
Cervical Foraminotomy
Cervical foraminotomy is a procedure carried out in conjunction with disc surgery. The foramen (openings for the individual nerve roots to pass from the spine) may become narrowed because of disc impingement, intervertebral collapse, and spondylolisthesis. The surgical widening of the foramen is an attempt to relieve the pressure on the nerve roots.
While it often is performed in conjunction with an anterior cervical discectomy and fusion, it can also be performed as a standalone procedure via a posterior approach. When performed via a posterior approach, it is done in minimally invasive fashion through a small incision and with the use of an operating microscope.
Cervical Laminoplasty
Cervical laminoplasty involves cutting the lamina completely on one side and partially on the other so that the lamina can be opened up using the partially cut side as a hinge. This preserves the roof of the spine so it can protect the spinal cord while still taking the pressure off of the spinal cord.
Microdiscectomy
A discectomy refers to the excision of the intervertebral disc material that may be described as herniated, implying it is “bulging” or “ruptured” through the ligaments. If the central fragment of disc material has torn through a hole in the ligament, it is called an extruded fragment or extruded disc. The term herniated nucleus pulposus (HNP) is a catchall phrase for all of these conditions. The prefix “micro”—in microdiscectomy—is used to denote that the operation is done through use of an operating microscope where Dr. Kim will employ microsurgical techniques.
Minimally Invasive Spine Surgery
Minimally invasive spine surgery is an alternative to traditional open surgery. The goal of minimally invasive spine surgery is to cause less harm to surrounding muscle, ligament, and tissue in order to achieve the same objective. In many cases, this may lead to less blood loss, less postoperative pain, and a faster recovery. There are some pathologies that are amenable to a minimally invasive approach. Surgery is a last resort. In cases where Dr. Kim is confident that your issue can be safely addressed surgically, Dr. Kim may offer a minimally invasive approach.
Endoscopic Spine Surgery
Endoscopic spine surgery is a minimally invasive procedure that can help relieve lower back pain caused by conditions such as a herniated disc and spinal stenosis. Due to the small incisions that are made, there is typically a smaller risk of infection and scarring. The chance of soft tissue and bone trauma is also reduced. Following the procedure, patients often see less postoperative pain and a faster discovery time than other approaches.
Spinal Fusion
A spinal fusion is a surgical procedure to permanently join bone by interconnecting two or more vertebrae in order to prevent motion, to relieve pain, and prevent further degeneration by restoring alignment.
Scheuermann Kyphosis Correction
Dr. Holger Scheuermann described a clinical finding characterized by rigid developmental thoracic kyphosis. This condition would later be called Scheuermann’s kyphosis. The etiology of Scheuermann’s kyphosis remains unclear, but biomechanical factors contribute to the development and progression of the deformity. The natural history of Scheuermann’s kyphosis is benign and only in rare cases can it lead to neurologic deficits. However, patients with moderate to severe Scheuermann’s disease do have more back pain. Symptomatic curves greater than 75 degrees usually warrant surgery. Other indications include painful curves, progressive curves, unacceptable appearance, restrictive pulmonary disease, and neurologic deficits. There is a potentially significant impact of the spinal deformity on a patient’s self-esteem and self-perception.
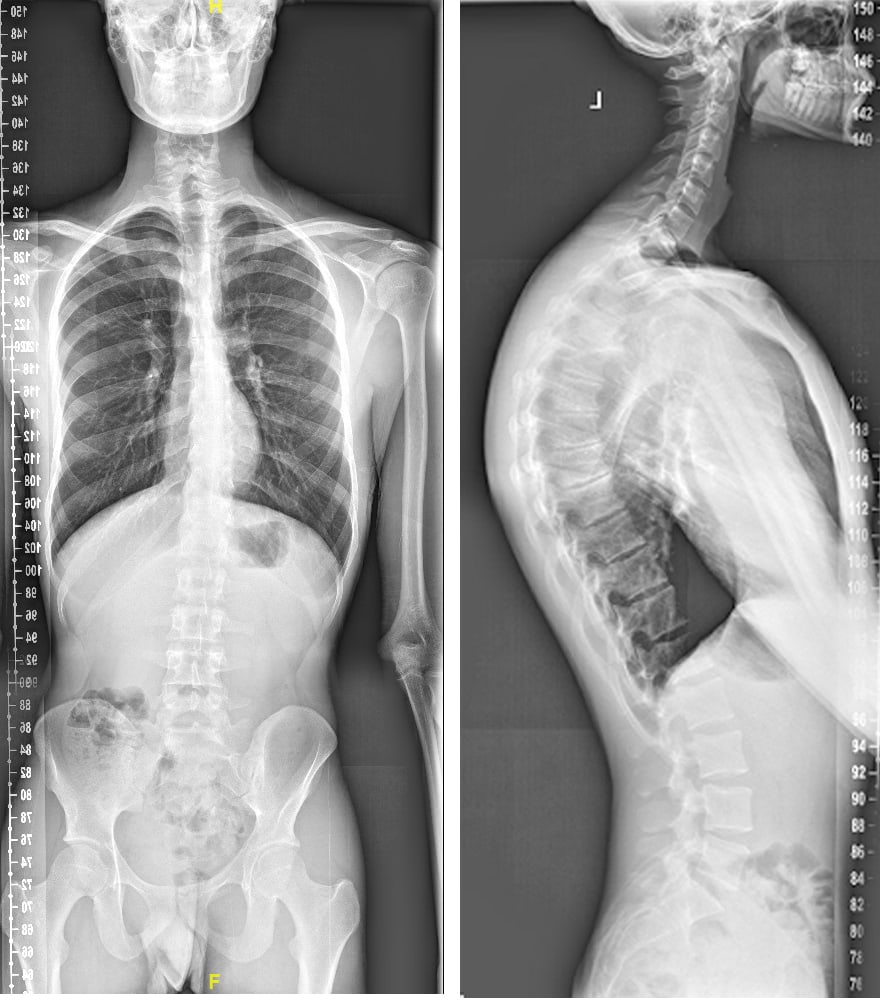
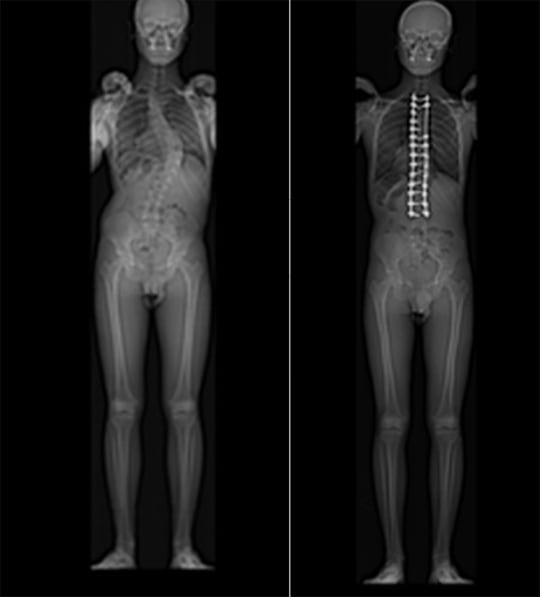
Preoperative X-Ray Scheuermann Kyphosis
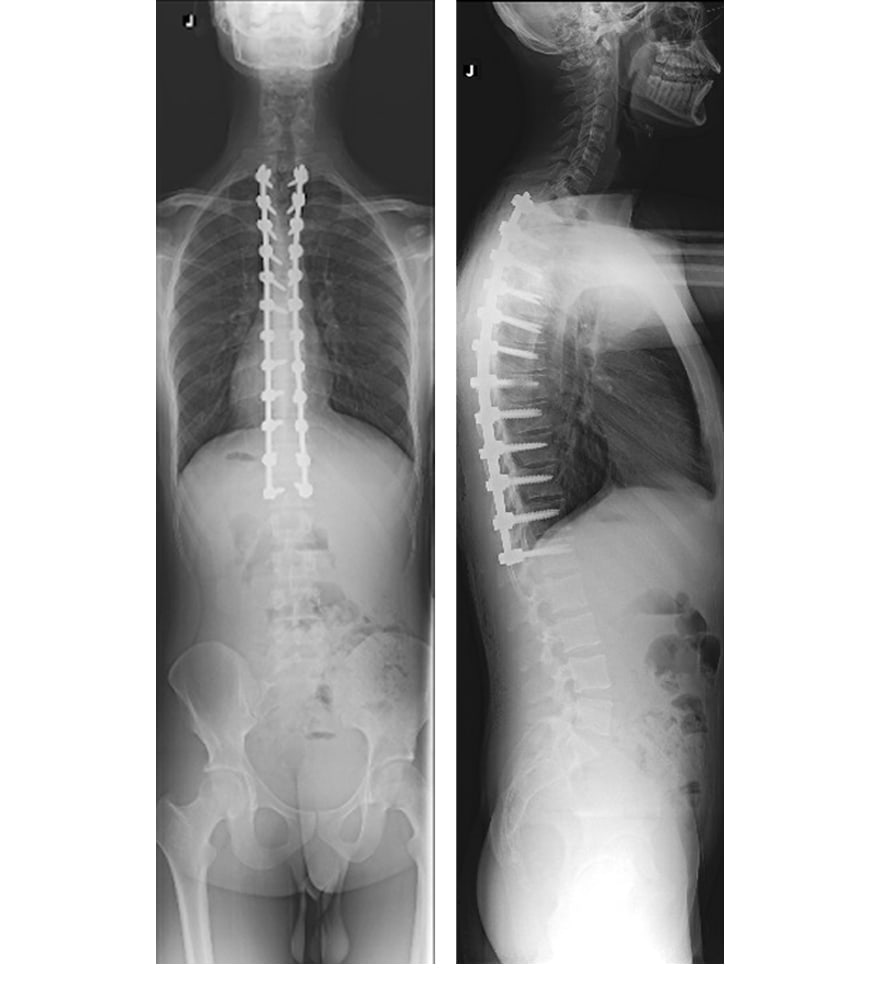
Postoperative X-ray Scheuermann Kyphosis
Kyphoscoliosis Correction
Kyphoscoliosis refers to cases where the deformity also includes a kyphosis with scoliosis. The vertebral bodies may be rotated and attenuated. This can lead to a deformity that can be seen not just from the front, but also from the patient’s side. These deformities require a multidisciplinary team at a tertiary care health system to treat.
Your team will consist of the spine surgeon, geneticist, internist or pediatrician, pulmonologist, endocrinologist, rehabilitation and physiatry physician, physical and occupational therapist, anesthesiologist, neurologist, radiologist, critical care intensivist, and nurses.